This article is a follow-up to the Tenovi Talks webinar: How to Add RPM to CCM Strengthening Patient Care. Thank you to everyone who joined the recent Tenovi Talks webinar session. Many questions came in concerning RPM and CCM services that we were not able to address during the live conversation. This article highlights the most meaningful takeaways and answers some of the questions that came up during the discussion.
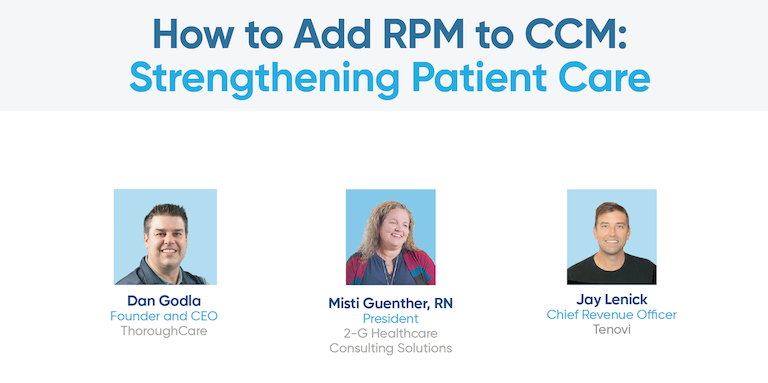
The webinar featured:
- Misti Guenther, RN, President, 2-G Healthcare Consulting Solutions
- Dan Godla, Founder, ThoroughCare: LinkedIn contact
- Jay Lenick, CRO, Tenovi: LinkedIn contact
RPM and CCM Services: Why Add RPM to CCM
Panelists emphasized that remote patient monitoring strengthens chronic care management by providing objective data between phone calls and office visits, giving care teams the ability to intervene before complications escalate. According to Misti Guenther, real-time vital sign monitoring has been key to preventing avoidable hospitalizations.
One of her examples involved an 81-year-old patient with newly diagnosed AFib, CHF, hypertension, kidney failure, and anemia. After enrollment into CCM and RPM and daily monitoring with a Tenovi blood pressure monitor and scale, the patient has had no ER visits and no unplanned hospitalizations.
Another patient story involved identifying concerning trends through RPM. A cardiologist directed the patient to come in immediately, resulting in a lifesaving bypass surgery that was scheduled instead of emergent. As Guenther explained, the outcome was possible because the care team had real data, not assumptions.
Where to Start When Adding RPM to CCM Services
Many attendees asked about the right place to begin. The recommendation from the panel was clear: start by reviewing your patient population.
- Identify chronic conditions where ongoing vitals matter, such as hypertension, COPD, CHF, diabetes, obesity, or multiple comorbidities.
- Use analytics to determine which patients would benefit most from consistent monitoring.
- Engage providers early in the process.
Guenther noted that the most successful workflow involves building a care team capable of communicating with patients consistently. RPM works best when paired with education and coaching, not just measurement. Patients often describe the process as reassuring. They appreciate knowing that someone is monitoring their health in real time instead of waiting until the next office visit.
RPM and CCM Services: Challenges and Solutions
Many patients report feeling like they are receiving VIP-level attention because the program creates continuous touchpoints. A consistent challenge is that once patients begin to feel better, it may be thought that they no longer need the service. Guenther shared that educating patients on the long-term value of RPM helps maintain adherence.
Another common concern is device deployment and connectivity. For rural regions, cellular-enabled devices reduce barriers by eliminating Wi-Fi requirements. Reliable transmission ensures care teams can react quickly to trending values.
2026 RPM Billing Updates: What to Know
Many questions focused on billing changes for 2026. Dan Godla explained that CMS has introduced new CPT code updates allowing billing for lower measurement frequency and lower care management time thresholds.
- Providers can bill for two to fifteen days of readings per 30-day period under a new code projected to reimburse at the same level as 16 readings.
- Providers can now bill at 10 minutes of clinical review time per month instead of the previous 20-minute minimum.
- These additions expand eligibility to patients who may only need weekly measurement.
Godla cautioned that providers should continue to document clearly. The new codes should support edge-case patients, not reduce engagement expectations.
Q&A: RPM and CCM Services
Q: Which patient population should programs begin with?
Hypertensive patients are often the first group, and many programs begin by reviewing unstable hypertension. Diabetic, CHF, COPD, and obesity patients also demonstrate strong benefit. RPM use cases continue to grow as healthcare increasingly shifts to connected patient-centered care.
Q: What is the typical time to launch RPM within an existing CCM program?
Most groups that already operate CCM can activate RPM quickly once patient selection and device workflows are aligned.
Q: How do you maintain patient participation long term?
Education, frequent communication, and clear expectations. Patients who understand the purpose are more consistent and engaged. Notification reminders and Tenovi Gateway visual cues can help increase adherence to daily measurements.
Q Can RPM and CCM be billed together?
Yes, CCM and RPM can be billed for the same patient as long as the time and activities counted toward each service are distinct and do not overlap.
Q Does CCM require a once-a-year in-person visit?
Yes, CCM, RPM, and RTM require that a patient has had a billable visit within the past 12 months.
Q How much is a device?
Tenovi provides customized pricing based on the type of device and program volume. An RPM expert can walk you through pricing. Please book a meeting to learn more.
Watch the Replay
If you missed the session or would like to review it with your team, the full webinar recording is available to download.